Think you need an injection for your hip pain? We suggest you read this first…
We frequently treat patients with lateral hip pain and understand the effect that pain in this region have on daily life and sleep. Lateral hip pain can make everyday activities such as walking, climbing steps or stairs, sitting, or even lying on your side difficult and painful. To effectively manage lateral hip pain, a good understanding of the underlying anatomy is required (firstly through obtaining an accurate diagnosis by your Physiotherapist), and through a combination of treatment approaches including education, activity modification and specific exercise therapy, significant improvements can be achieved over time.
In this blog we’ll discuss the most common cause of ‘Gluteal Tendinopathy’, with a specific focus on the most evidence-based approach to rehabilitation following a recent research paper by several experts in this area (Mellor et al 2016).
Lateral hip pain (e.g. pain located over the outside of your hip) is common, persistent and can be extremely debilitating. Lateral hip pain generally presents in the form of an underlying Gluteal Tendinopathy and is most common in women aged 40-60 years, but also effects a substantial proportion of the general population, with reports ranging from 10-25% (up to 1 in 4 people!).
Historically, lateral hip pain was often called to ‘Bursitis’ (referring to ‘Trochanteric Bursitis’) where by inflammation of the bursa (a small fluid filled sack that functions to reduce friction between the tendons and bones) was thought to be the primary source of lateral hip pain.
With increased research in this area alongside advances in medical imaging (e.g. MRI findings), we now know that most commonly, the source of lateral hip pain is tendon changes to the Gluteus Medius and/or Minimus Tendon, right where the tendons insert onto the hip bone. While inflammation of the bursa may or may not be present, this is often a secondary result of the underlying Gluteal Tendinopathy.
The differences in the pathology of the underlying condition are noteworthy, with ‘bursitis’ (‘itis’) referring to tissue inflammation: a process of increased tissue sensitivity and healing, while a ‘tendinopathy’ refers to structural disorganisation of the tendon and therefore reduced capacity to bear load (e.g. force).
This changes the treatment approach from passive therapies like ice, massage, rest and anti-inflammatory medications (to name a few), to more active approaches including education on condition management and modification of everyday activities (e.g. avoiding activities that consistently increase your pain) and a targeted exercise programme to strengthen weak gluteal muscles, which is a common finding in people with a Gluteal Tendinopathy. While the exact mechanisms are not fully understood, resistance training exercises (e.g. in this case specific to the gluteal muscles) is believed to stimulate tendon remodelling and therefore increase the ability to tolerate load.
Recently, a key research paper compared the effectiveness of three management approaches for individuals with a Gluteal Tendinopathy (Mellor et al. 2016). The researchers recruited 204 people diagnosed with a Gluteal Tendinopathy and randomised them to three groups, receiving either:
See a summary of the study results here (BMJ 2018;361:k1662):
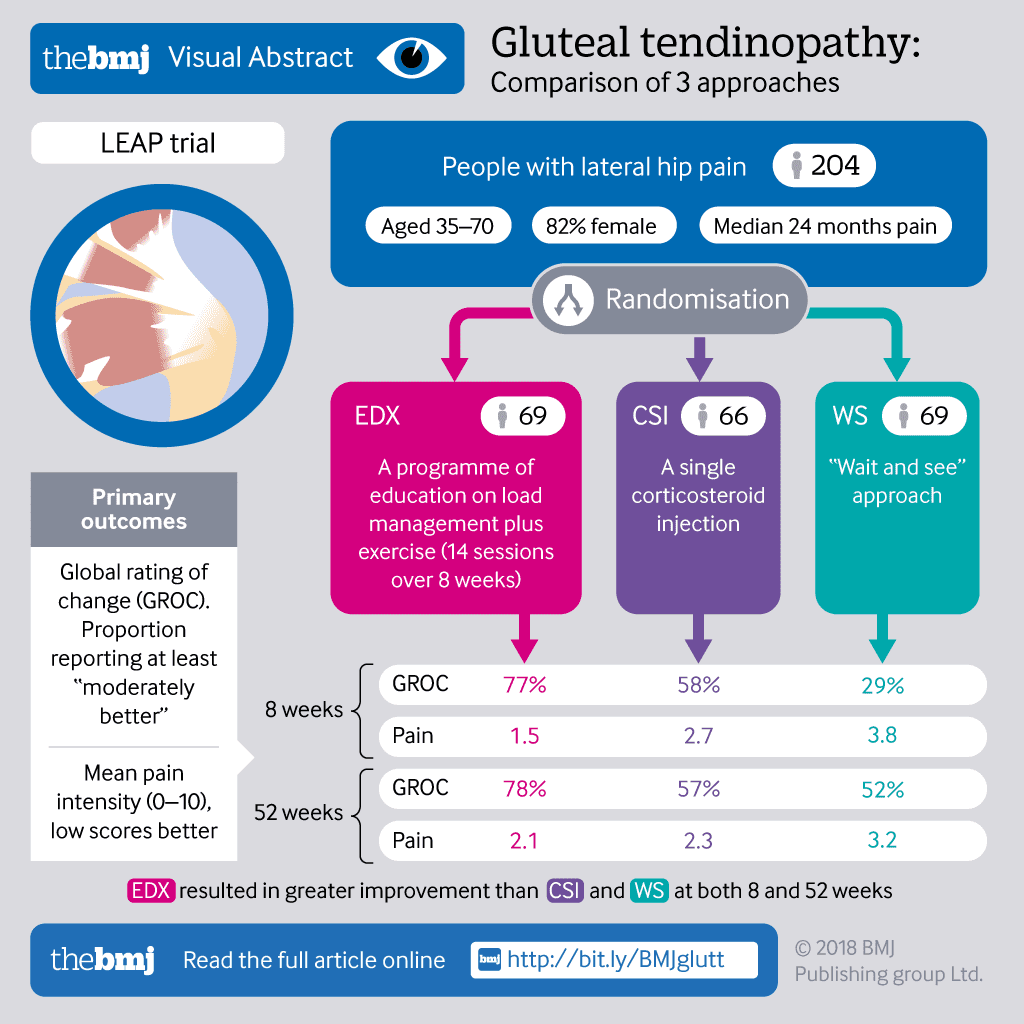
Findings revealed after both eight weeks and 12 months (short and long term respectively), greatest improvements in overall condition outcome (‘GROC’) and pain reduction (‘Pain’) were found in the group receiving education, load management advice and exercise therapy (EDX), compared to both corticosteroid injection (CSI) or the wait and see (WS) control group.
The results of this study tell us a few things.
Firstly, in the patients studied (diagnosed with a Gluteal Tendinopathy) active management is effective in both the short and long term at reducing pain and improving overall condition outcomes (as rated by you), and that active management appears to be more effective than corticosteroid injection or simply waiting for the condition to improve over time.
Most importantly, education and load management advice were delivered by a Physiotherapist with knowledge in this area, while exercises were prescribed specifically to strengthen the gluteal muscles and tendons and progressed gradually over time.
At Move for Better Health, we understand that lateral hip pain can be complex, and that a detailed assessment, accurate diagnosis and long-term management plan (specific for you) is required to get you back to living your best and most active life. If you do indeed have Gluteal Tendinopathy, a management plan consisting of education, load management and supervised exercise therapy is considered evidence-based and best practice. Of course, each pain presentation is unique to the individual, so discussion of other treatment options (such as corticosteroid injection) with your physiotherapist is always encouraged.
To assist in recovery, Move for Better Health offer a range of supervised exercise classes allowing you to complete your tailored exercise programme under direct supervision. For further information on exercise options and tendinopathy treatment, click here.
Mellor, R, Bennell, K, Grimaldi, A, Nicolson, P, Kasza, J, Hodges, P, Wajswelner, H & Vicenzino, B 2018, ‘Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial’, BMJ, 361, k1662. doi:10.1136/bmj.k1662.
Allison, K, Vicenzino, B, Wrigley, TV, Grimaldi, A, Hodges, PW & Bennell, KL 2016, ‘Hip Abductor Muscle Weakness in Individuals with Gluteal Tendinopathy’, Medicine and Science in Sports and Exercise, vol. 48, no. 3, 346-352. doi:10.1249/MSS.0000000000000781.
Grimaldi, A, Mellor, R, Hodges, P, Bennell, K, Wajswelner, H & Vicenzino, B 2015, ‘Gluteal Tendinopathy: A Review of Mechanisms, Assessment and Management’, Sports Medicine, vol. 45, no. 8, 1107-1119. doi:10.1007/s40279-015-0336-5.
Dietitian Role Description Move for Better Health is seeking a new dietetics provider for our clinics. We...Read More
At Move for Better Health, one of our key goals is to help you move more. We...Read More
At Move for Better Health, we understand that optimising your health over the life span can be...Read More